Injuries
to the fingers and hands consist of:
Overuse
syndromes:
- Tendovaginitis
- Trigger finger
- Dupuytrens
Injuries:
- Pulley injuries - (click here for more information on pulley injuries)
- Lumbrical Tears
- Collateral ligament and Capsular injuries
- Wearing of rings when climbingPlease note, for all injuries, treatment for the acute phases (first 24-72 hours) is always to follow the POLICE guidelines (see previous blog post)
Tendovaginitis
Anatomy
Tendovaginitis
isn't just a dirty sounding word, it's what climbers commonly refer
to as tendonitis. Tendonitis is actually the inflammation of a
tendon, whereas tendovaginitis is inflammation of the tendon sheath.
A
stress exerted to the tendon sheath via increased friction to the
tendon results in inflammation.
This
inflammation restricts the tendon moving through the sheath which
impairs movement of the tendon and in turn causes more irritation.
The body responds by increasing the fibrin to the area to aid
lubrication of the joint, which only increases the inflammation and
irritation and causes a vicious circle.
This
scenario over a lengthy period can cause adhesions to the tendon
sheath and narrowing of the space in the tendon sheath, meaning that
the tendovaginitis becomes inflammed easily and so creates a
reproduction of symptoms.
Tendovaginitis
for climbers can occur in the fingers, or forearm
Causes
- Crimping (due to the 90 degree angle of the finger joints resulting in the highest stress through the tendons and associated sheaths)
- Repetitive one-sided stress (e.g. campus board)
- Climbing tired
- Climbing without adequate rest periods
Symptoms
- Dull ache in the hand
- Swelling in the affected joint area
- Pressure sensitivity of the flexor tendons
- Pain and strain during motion
- Grinding in the tendon sheath
Treatment
- Rest and immobilization (POLICE principles)
- Returning to climbing once the swelling and acute symptoms have subsided easily and gradually
- Anti-inflammatories
- Corticosteriod injection (depending on severity)
- Tape
- Acupuncture
- Electrotherapy
Trigger
Finger
Anatomy
Trigger
finger is nicely displayed in the picture above. It's characteristic
symptom is finding the finger stopping, then snapping past a
particular point.
This
nodular thickening or knot is caused by chronic overuse creating
micro-tears to the tendon that has formed scar tissue excessively
around the injury site. It is then this formation of scar tissue that
creates a blockade when the tendon is trying to pass through a pulley
and creates the distinct trigger snap.
Causes
- Chronic overuse of fingers
- Chronic tendovaginitis
- Serious tendon tear that has healed with a lot of scar tissue
Symptoms
- Distinctive snapping past a point when extending the fingers.
- Sensitivity or pain upon pressure to the tendon
- Palpable knot of the tendon
- Tendovaginitis symptoms
Treatment
- Stress reduction
- Vigorous massage to the knot
- Corticosteroid injection to tendon sheath
- Surgical intervention with splinting of A1 pulley
Dupuytrens
Anatomy
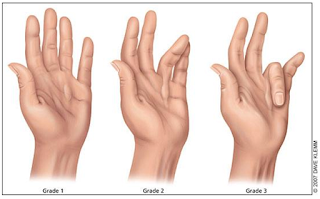
Dupuytrens is a heriditary condition that causes
thickening to the palmar fascia which causes the flexor tendon to be
shortened. Some report it usually affects the ring, middle and little
finger, sparing the thumb and index.
Initially, only nodule can be visible, but it can
spread and create a contracture as shown below.
Causes
Dupuytren’s disease often starts with nodules in
the palm of the hand and it can extend to a cord in the finger. The
palmar fascia becomes abnormally thick due to the fact that there is
a change of collagen type. Normally, the palmar fascia consists of
collagen type
I, but if a patient has Dupuytren’s disease, the collagen type
I changes to collagen
type III, which is significantly thicker than collagen type I.
However, the root cause of the condition is
unknown, therefore there is no “cure”, as such.
There is some evidence that the Dupuytren's may be
hereditary, but some risk factors have been identified:
- Men higher risk than women
- Over 40's
- Family history (60-70% of those with Dupuytren's has a family history of the condition)
- People with liver cirrhosis (linked with alcoholism)
Unproven but suspected is repeated micro-trauma,
possibility of occupational relationship, trauma and diabetes.
No definitive evidence has been found that links dupuytren's
with rock climbing specifically, although the repetitive stresses on
the fingers could be a factor.
Logan et al (2005) have found that 19.5% of 550 rock climbers in the UK had developed Dupuytren's, and that those with the disease climbed at a higher intensity, and that an earlier onset of the disease was found compared to the general population. So, coincidence or not, there does seem to be a higher incidence in a rock climbing population.
Logan et al (2005) have found that 19.5% of 550 rock climbers in the UK had developed Dupuytren's, and that those with the disease climbed at a higher intensity, and that an earlier onset of the disease was found compared to the general population. So, coincidence or not, there does seem to be a higher incidence in a rock climbing population.
The prevalence of Dupuytren's is also on the rise
in young climbers, and in comparison, is rare in young non-climbers.
Symptoms
- Nodular soft tissue scars in the palm
- Tenderness over this area
- Fixed flexed position of finger
Treatment
As previously mentioned, there is no cure for
Dupuytren's, but there is treatment methods to prevent the condition
getting any worse.
In it's early stages, Dupuytren's can be broken
down by vigorous massage over the affected area to break down the
scar tissue (anecdotal evidence only).
Radiotherapy treatment may also help.
However, I have found via personal experience that
the visible nodule of a Dupuytren's contracture is just the tip of
the iceberg, as it can actually be hiding a much deeper level of scar
tissue that is unseen without the use of ultrasound or other
diagnostic imaging tools.
If Dupuytren's progresses too far, then the only
option for regaining functional use of the hand is surgical
intervention. This can remove the scar tissue formed, however can
lead to a long period of no climbing, and the recurrence rate is
high.
Recently, a collagenase enzyme injection has been
developed, for non-surgical approach, but again, recurrence rate is
very high, but reports show that the recurrence is not as severe as
the original contracture. This also leads to 4 months of rehab and
using of night splints.
It must be noted that, although the lack of
substantial trialled evidence is obvious, there is a great deal of
anecdotal evidence that suggests that taking glucosamine supplements
accelerates the contracture process associated with Dupuytren's
disease (See Arthitis Research UK or Dupuytren Online)
Lumbrical
Tears
Anatomy
The lumbricals are muscles that are between your
metaphalangeal joints. They flex the metocarpalphalangeal joints
whilst extending the interphalangeal joints, performing the motion
pictured below.
Unlike most muscles, these attach to the flexor
digitorum profundus tendons and and distally to the extensor
expansions. They are fan shaped muscles.
The third and fourth lumbrical are the ones most
susceptible to injury, due to them both being bipennate and
originating from the flexor tendons.
Causes
When using a one finger pocket, normally, the
other fingers not in use are flexed maximally. If using a pocket with
the middle or ring finger, this causes a shift in the flexor tendons
and increases the distance between the origins of the lumbrical
muscle, therefore causing a disruption or tear in the muscle belly.
Symptoms
An audible snap (not too dissimilar to a pulley
rupture) with severe pain and swelling in the finger and palm.
Painful on palpation over the flexor tendons in the palm.
Holding a one finger pocket with the affected
finger results in severe pain in the palm, yet buddying up on two
finger pockets is painless.
This injury can be seen on ultrasound for accurate
diagnosis
Treatment
- Buddy taping middle and ring finger
- Moderate stretching programme of middle finger forced to flexed, ring finger forced into extension, and vice versa
- Preventing use of one finger pockets (at least until after 2-4 months)
Maximum strength in the injured finger may not
fully return, but due to the nature of the buddying up of fingers in
a painless symptom, climbing can continue for the injured party.
Further reading: Schwiezer 2003
Capsular
and Collateral Ligament Injuries
Anatomy
At each finger joint, between the interphalangeal
joints, there is a joint capsule that houses the synovial fluid for
the joint. Also, there are ligaments on each side of the joint called
the collateral ligaments.
Sometimes
an osseous lesion may occur (which I believe is a tumourlike boney abnormality) and an X-ray needs to be performed to rule this out as a cause of injury to the ligaments or capsule)
Causes
When using a crack or two finger pocket and
twisting, this can damage the structures mentioned above. Due to them
being linked, damaging one inevitably damages the other. Damaging the
ligament can be classified as a Grade I, II, or III.
They can also occur from dyno-ing and failing to
remove a finger from the starting pocket and catching it in an
upwards motion.
Symptoms
- Decreased mobility around the affected joint
- Pressure sensitivity
- Joint instability
- Swelling at the joint
Treatment
- Immobilization
- Splint
- Buddy taping
- Gentle stretching in the later stages
All
are designed to prevent instability around the joint.
Further reading: click here
Wearing
Rings When Climbing
Please
do not wear rings or any jewellery when climbing. I get you're
married or have a nice watch and want to show it off and are very
proud of it, but please take it off when climbing.
Worse
than a telling off from your wife while entail, such as incidents
like this (please note, gruesome pictures below)
Sorry, I can't do it, the pictures even give me
the heebie-jeebies! If you have a grotesque side, you can click here
for some images (if you do wear a ring while climbing, and think I'm
talking rubbish, please click the link – you need to understand the
seriousness of the situation.)
What makes it worse, too, is that the damage
caused by this “degloving” of the finger is very difficult to
repair.
Others
There are other injuries and conditions that affect the fingers for climbers, such as ganglions, tendon strains, fractures (including epiphyseal fractures), amputation and abcesses. However, I feel these are less common and, unless there is the demand, I won't blog about them (or at least have no aims too at the moment apart from epiphyseal fractures).
Let me know if you want me to discuss these points though.
Others
There are other injuries and conditions that affect the fingers for climbers, such as ganglions, tendon strains, fractures (including epiphyseal fractures), amputation and abcesses. However, I feel these are less common and, unless there is the demand, I won't blog about them (or at least have no aims too at the moment apart from epiphyseal fractures).
Let me know if you want me to discuss these points though.
References
Schoffl VR, Schoffl I 2007 Finger pain in rock climbers: reaching the right differential diagnosis and therapy. Journal of Sports Medicine Physical Fitness 47:70-78
Schwiezer A 2012 Sport climbing from a medical point of view. Swiss Medical Weekly 142: w13688
Schwiezer A 2003 Lumbrical tears in rock climbers. Journal of hand surgery 28B(2): 187-189
Logan AJ, Mason G, Dias J, Makwana N 2005 Can rock climbing lead to Dupuytren's disease? Br J Sports Med. 39(9):639-44.
Hochholzer T, Schoffl VR 2006 One Move Too Many. Lochner-Verlag, GermanyArthitis Research UK
Dupuytren Online