So this post is to explore the other
problems with elbows – specifically "climber's elbow" –
a differential elbow pain to that of tennis or golfers elbow. Less
common than biceps brachii injuries but quite common in climbers.
Climber's elbow is caused by tendonitis
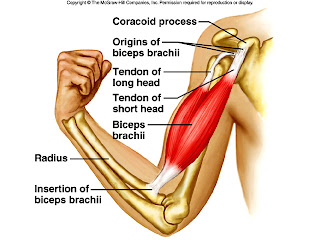
of the brachialis muscle. The brachialis muscle lies deeper than the
biceps brachii muscle and originates on the upper humerus and
attaches to the ulna.
Brachialis is a true flexor of the
elbow as it attaches to the ulnar (rather than attaching to the
radius which rotates over the top of the ulnar during pronation and
supination. N.B. Biceps brachii attaches to the radius)
Therefore, because of the broad origin
on brachialis and it's only function is to flex the elbow, the
brachialis can be considered the strongest elbow flexor.
This injury, if a gradual onset, is
most likely to be tendonitis. If there is pain in this area of the
elbow after a specific incident/fall, it could be a rupture of
ligaments or muscle tendons.
N.B. Pain in this area of the elbow, could be, as mentioned above, could be from biceps, from brachialis, or even from problems with the proximal ulna-radial ligament. Always worth getting these kind of problems checked out.
N.B. Pain in this area of the elbow, could be, as mentioned above, could be from biceps, from brachialis, or even from problems with the proximal ulna-radial ligament. Always worth getting these kind of problems checked out.
Also needing ruling out would be
shoulder / wrist / finger injuries or muscular imbalances.
Palpation
To try and identify the injured structures, you can try and palpate the painful area.
The brachialis tendon must also be
palpated for tenderness during elbow flexion, as both the biceps and
brachialis flex the elbow.
The brachialis muscle and its tendon are
palpated where they insert at the tuberosity of the ulna and the
coronoid process of the ulna.
Like the biceps, the distal end of the
muscle and/or the insertion of the tendon would be tender with
injury.
Supination of the hand would not necessarily affect the
brachialis tendon, helping to further differentiate between the two
muscles.
Symptoms
- Deep elbow pain (not superficial like tennis/golfers elbow generally is)
- Pain on anterior (front) elbow (note, this could be due to a biceps brachii injury)
- Swelling around the elbow or above the elbow (in the cubital fossa)
- Inability to bend elbow comfortably

Cause
Brachialis tears normally occur during a forceful contraction
or a forceful hyperextension while climbing. Complete tears are associated primarily with elbow
dislocation.
Tendonitis is normally caused by strain
from sudden increase in training, overuse or repetitive elbow bending
or forced, excessive elbow straightening (hyper-extension).
Treatment
Full rupture = surgical intervention would be required.
For a partial tear:
- Control inflammation in the acute phase – see POLICE Principles
- Rest
- Dep tissue frictions / Massage
- It has also been suggested that traversing may irritate the brachialis, so consider limiting this.
- If a tendonitis, the research suggests eccentric biceps curls (lowering of a weight in the curl position), however, I've found anecdotally that in the hammer position with your thumb pointing upwards works better.
- Exercise progression from isometrics to eccentric to concentric strengthening, ensuring all are pain free, progress from isometrics once full range of movement around the elbow is achieved
Prevention
As usual, warming up is a key
prevention method
Ensure adequate recovery time between climbing days
All-round strengthening of rotator
cuff, biceps and brachialis can maintain a good strength all round to
correct any kind of muscle imbalances.
Triceps can also need
stretching/strengthening depending on the imbalance.
Stretching of lattimuss dorsi and
biceps
Technique when performing pull-ups etc
or when climbing i.e. making sure you lock with your lats by keeping
your elbow close to your body. Try not to chicken-wing (see below)
In the bottom row of pictures, you can see the correct form for pull-ups, with the elbows tucked in
In the top row, the elbows are "winging", which makes you more prone to injury
Also note, don't snap your elbows straight when lowering from a pull-up, control the movement down.
Avoid:
- pull ups with weights – your working to body strength – why do you need to be able to do pull-ups with weights?!
- descending bachar ladder
- down climbing campus board
- no snapping back of elbows during climbing/pull ups
And if your wondering where I got the lovely t-shirt, go to climberagainstcancer.org
References
Live Strong article
Miller KJ 2013 Climber's Elbow: Diagnosis and
Conservative Treatment Protocols. Dynamic Chiropractic Vol. 31, Issue 01