So I'm going to take you back to
ancient times, where Gods ruled the lands, and the Greeks invented
the Achilles heel! This weeks post is going to focus on Achilles
Tendinopathy.
Other common rock climbing foot issues
will come in a later post.
Achilles tendon anatomy
Movements of the Achilles

Function
The Achilles tendon supports 6-15 times
your body weight and provides spring like action.
Tendonitis/tendinosis/tendinopathy,
what is the difference?
Tendonitis – inflammation
Tendinosis
– chronic tendinopathy
Tendinopathy – a disorder of the
tendons – an umbrella, catch-all term
Obviously, depending on -osis/-itis
depends on the management strategies (to counter the inflammatory
process or not).
The common consensus is that these
conditions are a tendinosis rather than a tendonitis.
Enthesopathies
The entheses is where the tendon
attaches to the bone, and an achilles tendinopathy that occurs within
the first 2cm of the tendon attachment to the calcaneus is an
enthesopathy.
Differential
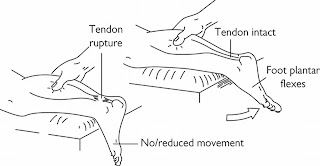
- Rule out complete tendon rupture using the calf squeeze test. See above picture.
- Posterior ankle impingement
- Os trigonum syndrome
- retrocalcaneal bursitis
- Posterior Tibial Tendon Dysfunction
- Haglund's deformity
However, to
discuss what all of these things are would take a whole blog post
unto itself, so I'm just going to leave it there!
Symptoms
- Pain in the heel/around the tendon
- ?swelling - if a tendinitis
- ?heat - if a tendinitis
- Painful to touch or on movement
- Early morning stiffness
- Difficulty standing on your tip-toes (/single leg stress/repetitive/hop)
Causes
Tendinopathy:
- Repetitive strain on tendon
- overuse
- inappropriate footwear
- poor technique
- high-arched foot
- increase intensity in training regime
- lots of jumping
- tight calves
- excessive inversion or eversion
Achilles tendinopathy is more a problem for
runners or walkers, but can affect climbers, especially as many
climbers are mutli-sports persons.
Enthesopathies: compression of calcaneus from repeated platarflexion e.g. aggressive climbing shoes and/or dynoing etc. as climbing shoes with an aggressive heel, such as 5:10's, could cause this repeated compression on the calcaneus. (obviously, other aggressive climbing shoe are available!)
Treatment
If you suffer from the "5:10 syndrome" as mentioned above, you could try this method of editing your climbing shoes by Llanberis Resoles
NSAIDs....?
I mark this with a
question mark, because it depends on your school of thought –
whether it is a chronic overuse, or an inflammatory response. If you
find it is swollen, then NSAID's may well help, but there is a school
of thought that they may inhibit healing if used inappropriately.
There is also the
dangers of overuse of NSAID's, as listed in Risks of Ibuprofen post
Acute management (see
Management of Acute Injuries post) – again, may not be necessary if the tendinopathy is
not an inflammatory process. e.g. if you use RSI of the wrist as an
example.
GTN (Glyceryl trinitrate)
This is the same
as the spray commonly used for angina, but is utilised topically –
i.e. localised patch of GTN. However, the reasoning behind why it
works is unclear, and commonly patients exhibit headaches and/or a
rash as side effects.
Steroid
A corticosteriod
injection may help, but has been shown to only have a short term
pain-relieving effects, and not much else. Also, these injections may
increase the risk of tendon
rupture by weakening the tendon.
Surgical
A surgical
intervention is rarely required for Achilles tendinopathy, and would
always be a last resort. A very last resort!
There are other
such treatments such as extracorporeal shockwave therapy and
sclerosing injections, but they are rarely used.
The best bet is for physiotherapy, and using specific protocols, outlined below:
Physiotherapy
Mobilisations of
the Achilles tendon
Ultrasound – useful if the
tendinopathy is a tendonitis, as ultrasound can be used to reduce the
inflammation.
Protocols/Exercises
Eccentric – Alfredson et al 1998
Two types of Eccentric Exercises will
be used: (Refer to Photo A, B, and C)
- The calf muscle is to be eccentrically loaded with the knee straight.
- To maximize the activation of the soleus muscle, also performed with the knee bent.
- Perform each exercise 3x with 15 repetitions.
- Use your hand on the wall as a guide for balance
- Begin with weight bearing load, progression to backpack weight when patient can perform the
- exercise routine without pain or discomfort (Photo D). Advanced progression under therapist’s guidance may include resistance from weight training equipment such as a Smith machine or a squat machine.
Eccentric-concentric – Silbernagel et
al 2007
Timeframe
These exercises need to be performed regularly, and for a time period of at least 3-6 months if not much longer!
Why do these work?
Effectiveness of eccentric exercises
has been proved, however, there are differing theories on why it
works.
Some say it affects type 1 collagen and
production and, in absence of repeated aggravation, may increase
tendon volume over longer term. As such, this increase the tendons
tensile strength.
The repetitive stretching of the tendon
with a lengthening of the muscle-tendon unit may have an impact of
the capacity of the unit to effectively absorb load.
Another theory is
that it changes the mechanism of pain-producing nerves by an
alteration of neovascularisation (which is an increase of blood flow
to an injured area, and along with this, an increase in nerve fibres,
meaning increased pain), as the repetitive nature may damage these
nerves and vessels.
Exercising during rehab
Due to the length of rehab being
several months rehab, many patients ask “Do I have to stop
exercising?” Silbernagel et al 2007 found that if the pain in your
Achilles tendon does not exceed 5/10 on visual analogue pain scale
(VAS) (during or after sport), then it is ok to carry on with your
sport, whilst continuing with the exercise protocol.
Risk of rupture?
80% of ruptures completely asymptomatic
97% associated with underlying
pathology
As always, if in doubt, always seek advice from a professional!
References
Alfredson H, Cook J 2007 A treatment
algorithm for managing Achilles tendinopathy: new treatment options
Br J Sports Med. 41(4): 211–216.
Silbernagel KG, Thomeé R, Eriksson BI,
Karlsson J 2007 Continued Sports Activity, Using a Pain-Monitoring
Model, During Rehabilitation in Patients With Achilles Tendinopathy:
A Randomized Controlled Study. American Journal of Sports Medicine
35(6): 897-906
Alfredson H, Pietilä T, Jonsson P,
Lorentzon R 1998 Heavy-Load Eccentric Calf Muscle Training For
Chronic Achilles Tendinosis American Journal of Sports Medicine
26(3): 360-366